Pharma companies have been increasingly investing in developing targeted alpha therapies for cancer treatment, using alpha-emitting isotopes such as Ac-225. However, the current supply for Ac-225 is limited, and thus, companies are working towards securing their supply chain. The recent investment by Eli Lilly in isotope manufacturer Ionetix brings to light the increasing interest of large pharmaceutical companies in Ac-225 and its uninterrupted supply for their pipelines. Similar to Eli Lilly, several other companies have strategically invested in or partnered with manufacturers to ensure a guaranteed supply.
Ac-225 is pegged as a promising isotope for next-generation cancer treatment
Among the recent advances in cancer therapies, only a few have shown as much promise as targeted alpha therapies have. Targeted alpha therapies (TAT) involve using alpha-emitting isotopes to selectively target and destroy cancerous tissue without causing significant damage to surrounding healthy tissue. This is facilitated by the short range of alpha radiation in human tissue (less than 0.1 mm), which corresponds to less than 10 cell diameters. Moreover, they are characterized by high energy levels (5-9 MeV), which results in the selective destruction of malignant cells.
Several alpha-emitting isotopes are currently being explored for TAT, the most common among them being Ac-225, At-211, Pb-212, and Bi-213. Of these, Ac-225 (actinium-225) is considered the most potent medical-grade radioisotope as it has a high decay energy of 5.9 MeV and a half-life of 10 days. It is the isotope of choice in several clinical trials, with about 15 Ac-225-based ongoing clinical trials currently in the USA. However, despite having substantial potential for developing next-generation treatments in the cancer space, their adoption has been slow, given the short supply of the isotope.
Ac-225 is not naturally available and is derived from Th-229 (thorium-229), a byproduct of uranium-233 (U-233), which is a leftover from the production of atomic weapons in the 1950s and 1960s. The initial batch of Ac-225 has been supplied by the US Department of Energy (DOE). However, the supply cannot keep up with the growing demand for trials.
Isotope producers invest to accelerate Ac-225 supply in the future
Currently, there are two commercialized routes to produce Ac-225. As mentioned above, the first and traditional route involves separating Ac-225 from Th-229, derived from the US government’s legacy reserves of U-233. The US government holds about 453kg of U-233, of which only about 256kg is of high quality and will produce about 24g of medical-grade thorium.
The government had previously started a program that extracted a small amount (150mCi) of Th-229, which produced about 1.2 Ci of Ac-225 per annum, enough to treat 1,200 patients. However, in 2019, the US DOE entered into a public-private partnership with Terra Power and Isotek to downblend its stock of U-233 to extract Th-229, which can further be used to develop Ac-225. In 2021, TerraPower entered into an agreement with Cardinal Health, a US-based commercial alpha contract manufacturing organization (CMO), to develop and produce Ac-225 for drug development commercial sales. This will likely significantly improve the supply of Ac-225 in the long run.
The other route to produce Ac-225 is through cyclotron production, which involves irradiating a Ra-226 (Radium-226) target with a proton and knocking off two neutrons. Several isotope manufacturers are adopting this technology and are working on increasing their manufacturing capacity.
Niowave, a US-based supplier of medical and industrial radioisotopes, uses a closed-loop cycle to produce high-purity Ac-225 and other alpha emitters from Ra-226 using a superconducting electron linear accelerator. Similarly, Ionetix, a leading cyclotron technology innovator and isotope manufacturer, uses the same technology to produce Ac-225 and managed to produce its first batch of Ac-225 in June 2024. The company commissioned its first cyclotron at its current facility in 2023, while it aims to install and commission a second cyclotron there in early 2025. By 2025, it is expected that the company will be able to produce about 1Ci per week. The company also aims to establish another site in the USA for Ac-225 production in 2026.
While isotope manufacturers are strategically working to enhance the production of Ac-225 in the long run, the current supply, which is required to fuel the ongoing clinical trials using Ac-225, is quite limited. In 2024, the worldwide supply of Ac-225 is estimated to be about 2Ci per annum, which is merely enough to treat 2,000 patients.
Pharma companies invest in securing their Ac-225 supply chain
Given its currently limited availability and immense potential, leading pharmaceutical players are adopting various strategies to secure their Ac-225 supply to support their targeted alpha therapies drug pipelines. Several leading players, such as Fusion Pharmaceuticals, Telix Pharmaceuticals, and Bayer, are actively working on partnering with companies producing Ac-225 to overcome supply-related challenges for their trials. Recently, a leading pharmaceutical company, Eli Lilly, also joined the bandwagon and secured its supply of the actinium isotope.
Fusion, which has three Ac-225-based drugs currently under trial, was one of the first movers in this regard and has inked several partner agreements to ensure a smooth supply.
In December 2020, Fusion entered into a partnership with TRIUMF, Canada’s national particle accelerator center. In this partnership, Fusion would provide the latter with up to US$18.5 million (CA$25 million) to upgrade its production facilities and scale up production of Ac-225. In return, Fusion would receive preferred access and pricing to the resulting isotope.
In June 2022, Fusion collaborated with Niowave, a US radioisotope manufacturer. Under the agreement, Fusion would invest up to US$5 million in Niowave to further develop their technology to increase their production capacity of Ac-225. In return, Fusion will be guaranteed access to a pre-determined percentage of Niowave’s capacity of the resulting Ac-225, as well as preferred access to any excess stock produced.
In November 2023, Fusion entered into an agreement with BWXT Medical, a US-based supplier of nuclear components and a subsidiary of BWX Technologies. Under the agreement, the latter agreed to provide Fusion with a preferential supply of Ra-225 (parent isotope of Ac-225) and access to high-specific activity generator technology. This would enable Fusion to produce Ac-225 at its own manufacturing facility for use in clinical trials. In addition, BMXT Medical provides Fusion with predetermined amounts of its actinium supply needs under a preferred partner agreement.
Another leading radiopharmaceutical player, Telix Pharmaceuticals, entered into an agreement with Cardinal Health in May 2024 to supply Ac-225 globally.
Similarly, in February 2024, Bayer signed an agreement with PanTera (a Belgian radioisotope production JV created by Ion Beam Applications and SCK CEN) to secure large-scale production of Ac-225. PanTera uses both the Ra-226 and Th-229 production mechanisms to produce Ac-225. It is collaborating with TerraPower to supply Th-229.
Eli Lilly, the largest pharmaceutical company globally, has also recently invested in a nuclear isotope manufacturing company, Ionetix, in August 2024. Eli Lilly has made a US$10 million convertible loan investment in the company to secure its supply of Ac-225. Moreover, PointBiopharma, which was acquired by Eli Lilly in 2023, also had a previous US$10 million investment in Ionetix, resulting in Eli Lilly holding a total of US$20 million debt facility with Ionetix. The pharma giant has the option to convert this debt into equity when Ionetix’s valuation exceeds US$300 million.
These investments by Eli Lilly and Fusion Pharmaceuticals are rare cases where major pharmaceutical companies are investing up the supply chain to secure actinium availability for their cutting-edge drug pipelines.
EOS Perspective
While targeted alpha therapies are emerging as high-potential next-generation cancer drugs, they are plagued by supply constraints of alpha-emitting isotopes, especially Ac-225. Thus, companies seeing great promise in these therapies must work towards securing their supply of these isotopes to ensure the smooth running of their clinical trials.
In the past, large pharmaceutical companies such as BMS have had to halt enrolment in their clinical trials due to the non-availability of Ac-225. Such interruptions not only delay the entire clinical trial but also have significant cost implications and could jeopardize its overall success.
Considering these limitations, it is imperative that pharmaceutical companies with ongoing or planned Ac-225-based trials invest in ensuring a guaranteed supply of the isotope for the entirety of their trial and future production of the drug once approved. While several companies are merely entering into supply agreements with isotope manufacturers, others are taking it one step ahead and investing in their upstream suppliers. Moreover, some companies, such as Fusion and now BMS, are advancing towards building on-site production of Ac-225.
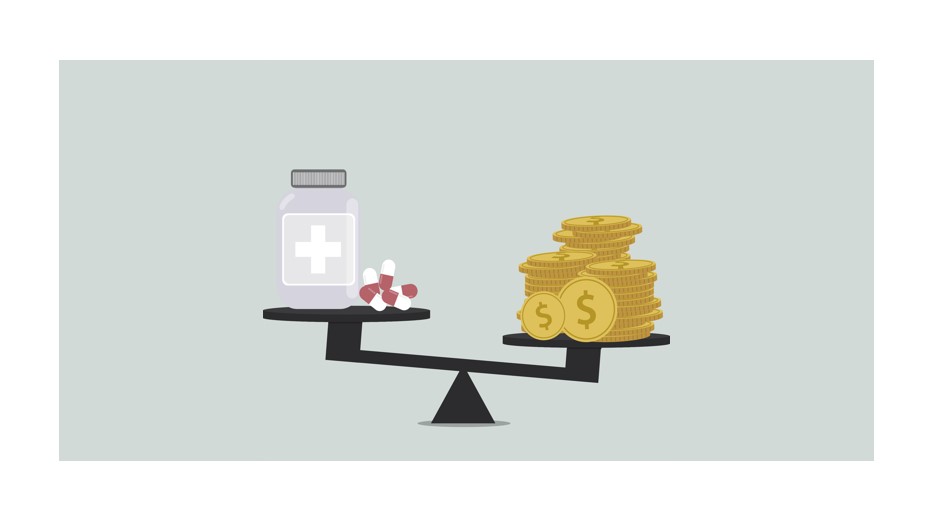
That being said, establishing a secure supply chain of Ac-225 comes with its own set of costs and risks. Most pharmaceutical companies are undertaking significant investments (ranging between US$5-25 million) to guarantee their supply of Ac-225.
However, as a cancer therapy, TAT is in the nascent stages of development, and most trials utilizing Ac-225 are still in either phase 1 or phase 1/2, far from FDA approval. Moreover, the only Ac-225-based trial in phase 3 is being conducted by BMS for neuroendocrine cancer and is currently halted due to supply issues. Given the nascency and early stages of development of this treatment, it is too soon to predict if these heavy investments into Ac-225 would result in the development of FDA-approved drugs and bring sufficient returns. This risk can have particularly dire consequences for small players.
Thus, while companies looking to develop targeted alpha therapies using Ac-225 must work to secure their supply, their level of investment must remain in sober relation to their size, pipeline, and financial position.